Why do my knees hurt from running?
The highly addictive activity of running is, to a large extent, very beneficial. Unfortunately, with each impact, large mechanical forces are passed from the foot systems through the ball of the foot, knees, thighs, hips, and back. It is the knees that are the most commonly affected part of the body when running. It is a very complex joint with many delicate structures. So you could say that they are the most susceptible part of the body to injury when running. They are responsible for up to 26% of running-related injuries (1).
The most common causes of knee pain and something about them
Pain can come suddenly, for example, with meniscus damage, muscle tears, or ligament or tendon ruptures. We refer to such injuries as acute, and you should see a doctor immediately. A larger proportion of knee injuries are chronic injuries, which occur over a longer period of time. The pain worsensover time, so diagnosis and recovery can take a long time. Their ranking is given by how often they occur.
Patellofemoral syndrome or runner's knee
What is runner's knee?
- It is chronic and the most common knee pain in runners.
Runner's knee: where does it hurt?
- The pain is localized in the anterior segment of the knee, directly behind the kneecap.
Causes of runner's knee
- The main cause is long-term overloading of the knee in the kneecap area. Running, stairs, jumps, squats and other repetitive movements with bending and stretching of the knee can be the cause.
Is anyone predisposed to runner's knee?
- The vast majority of people so affected are athletes who overuse the knee. But some people are just more prone to such an injury. This pathology is more common in women, in people with a false gait, in people with an unstable kneecap or a flaccid thigh muscle.
How long does it take to recover from runner’s knee?
- The duration depends on how early the syndrome is diagnosed. Easy cases may take a few weeks to recover, while other more severe cases may take months or years. The important thing is to return to training gradually and without pain.
How to treat a runner's knee?
- In any case it is a good idea to be examined by an orthopaedic doctor who can prescribe medication, orthopaedic aids, and rehabilitation. For medication, you may be given anti-inflammatory analgesics to relieve pain and inflammation, or perhaps corticosteroids. You might be ordered a brace too. But the most important thing is physiotherapy. You need to give the knee time off to recover, but at the same time stay moderately active and the right level is not easy to find. You have to load the leg gradually and over time, but never let the pain get worse even afterwards. As long as it doesn't hurt, you can stretch the knee in moderation, stretch it, even start squatting on it over time (2), (3).

Iliotibial syndrome (ITB syndrome)
What is ITB syndrome?
- This syndrome is one of the most common causes of chronic knee pain. These are painful pathological changes in the structures around the knee.
ITB syndrome: where does it hurt?
- The pain in this injury occurs on the outside of the knee. It is at the point where the iliotibial tract attaches, which is a ligamentous continuation of several muscles of the buttock and thigh. The pain typically comes with bending the knee and can hurt during or after activity.
Causes of ITB syndrome
- Many factors lead to the development of pain. A major contributor is the repetitive friction caused by bending and stretching the knee. The site of friction undergoes certain changes to which the abundantly innervated iliotibialtendon responds with pain. In addition, the influence of inflammation or enlargement of the extensor capsule cannot be ruled out.
Who is prone to ITB?
- Predisposed are people with shortened and very tight iliotibial tract or weak leg extensors. Together with risk factors in the form of many walked, run and cycled kilometres, iliotibial syndrome develops.
How long does it take to recover from ITB syndrome?
- As always, it is individual, but the pain typically goes away after 6-8 weeks of rest. Your return to training should look like starting with running over smaller distances, on the flat, and always taking at least a day of rest between runs. Only after 3-4 pain free weeks you can try increasing distance, intensity and run up and down hills.
How to treat ITB?
- Unfortunately, the treatment does not work immediately. It is necessary to give the injury a rest and start to gradually load it after the pain goes away. Icing is also effective. Stretching the ilitibial tract or massaging it with a massage roller is also effective. Anti-inflammatory drugs or corticosteroids are given only in severe inflammation. Of course, surgery is the last resort when the situation does not improve even after 6 months of rest (4), (5).

Rupture of the meniscus
What is menisci rupture?
- A meniscus rupture is a very unpleasant acute injury. It causes a partial or complete tear of the ligamentous cartilage that normally prevents friction between the femur and the tibia.
Where does menisci rupture hurt?
- Bolest typicky přichází náhle při pohybu v moment poškození menisku. Poté poměrně dlouho bolí při pokusu a zátěž. Bolest je výraznější na té straně kolene, kde se meniskus poranil. Často zranění doprovází otok.
What causes menisci rupture?
- The meniscus usually ruptures when it is overloaded during sports. Typically, during an unfortunate impact, an uncoordinated bounce during running or even a squat with high weight.
Who is prone to menisci rupture?
- It is easier to tear or rupture a meniscus that is already degeneratively altered by overuse. Thus, long-time runners have menisci slightly more prone to injury.
How long does it take to recover meniscus rupture?
- Unfortunately, full recovery of a ruptured meniscus takes months, in some cases even years.
How to treat meniscus rupture?
- Approaches vary depending on the severity and whether you are willing to undergo surgery. It is essential to discuss your situation with your doctor, who will present you with your options. It is possible to have the meniscus healed conservatively. This requires at least 3 months of rest, with the possibility of injections to promote healing. There are 2 surgical solutions. Either arthroscopically remove the meniscus, which was popular before, or arthroscopically stabilize the meniscus and allow it to heal. Stabilization of the injured meniscus, according to studies, comes out as the best option with the highest chance of the athlete still returning to running (6), (7), and (8).

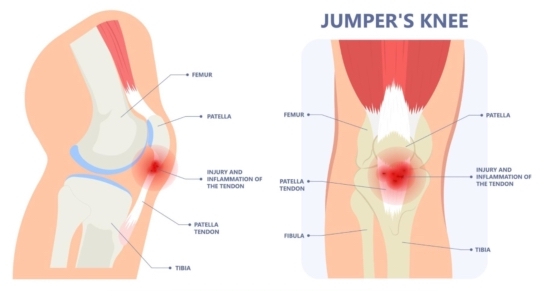
Patellar tendinopathy
What is patellar tendinopathy?
- It is a chronic injury of the tendon by which the thigh muscle attaches over the patella to the tibia.
Where does it hurt?
- Patellar tendinopathy typically hurts at the front of the knee and below the kneecap.
Causes of patellar tendinopathy
- The patellar tendon is extremely stressed during rebound, and prolonged overloadingis one of the main factors in the development of tendinopathy. The greatest degree of change occurs on the back side of the tendon. The tendon gets thicker but loses its mechanical properties.
Factors making you prone to patelar tendinopatia
- Poor foot posture, high weight and weakness of the thigh muscles are risk factors that contribute to patellar tendinopathy.
How long does it take to recover from patellar tendinopathy?
- In the majority of cases, with proper treatment, the pain completely disappears after 12 weeks.
Treatment of patelar tendinopatia
- The first and most effective treatment option is rehabilitation; surgery is not recommended for this injury. Relative rest should be maintained. However, with absolute rest, the tendon would atrophy, but with too much load, the tendon will not heal. Always consult a private physiotherapist can advise you on a specific rehabilitation exercise program, or a doctor can prescribe rehabilitation (9, 10).
References:
- Francis, Peter et al. “The Proportion of Lower Limb Running Injuries by Gender, Anatomical Location and Specific Pathology: A Systematic Review.” Journal of sports science & medicine vol. 18,1 21-31. 11 Feb. 2019
- Gaitonde, David Y et al. “Patellofemoral Pain Syndrome.” American family physician vol. 99,2 (2019): 88-94.
- Petersen, Wolf et al. “Patellofemoral pain syndrome.” Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA vol. 22,10 (2014): 2264-74. doi:10.1007/s00167-013-2759-6
- Hadeed, Andrew. and David C. Tapscott. “Iliotibial Band Friction Syndrome.” StatPearls, StatPearls Publishing, 23 May 2023.
- Khaund, Razib, and Sharon H Flynn. “Iliotibial band syndrome: a common source of knee pain.” American family physician vol. 71,8 (2005): 1545-50.
- Beaufils, P, and N Pujol. “Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus.” Orthopaedics & traumatology, surgery & research : OTSR vol. 103,8S (2017): S237-S244. doi:10.1016/j.otsr.2017.08.003
- Kopf S, Beaufils P, Hirschmann MT, Rotigliano N, Ollivier M, Pereira H, Verdonk R, Darabos N, Ntagiopoulos P, Dejour D, Seil R, Becker R. Management of traumatic meniscus tears: the 2019 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2020 Apr;28(4):1177-1194. doi: 10.1007/s00167-020-05847-3. Epub 2020 Feb 13. PMID: 32052121; PMCID: PMC7148286.
- Snoeker, Barbara A M et al. “Risk factors for meniscal tears: a systematic review including meta-analysis.” The Journal of orthopaedic and sports physical therapy vol. 43,6 (2013): 352-67. doi:10.2519/jospt.2013.4295
- Schwartz A, Watson JN, Hutchinson MR. Patellar Tendinopathy. Sports Health. 2015 Sep-Oct;7(5):415-20. doi: 10.1177/1941738114568775. Epub 2015 Jan 23. PMID: 26502416; PMCID: PMC4547110.
- Muaidi, Qassim I. “Rehabilitation of patellar tendinopathy.” Journal of musculoskeletal & neuronal interactions vol. 20,4 (2020): 535-540.
Photo sources:
- https://www.socalhip.com/wp-content/uploads/2022/01/Patellofemoral-Pain-Syndrome.png?fbclid=IwAR0n1_8u4ijobqf8mZMemsfNju5cyNGv7emRsN4gVbesNi7695vClJ2NzLY
- https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21967-iliotibial-band-syndrome?fbclid=IwAR1XSpvtjZo7oxiNhkAeJXaBir4SxMBHPAoVokuYT2bDICVEbIWvViEjeV8
- https://www.northeastspineandsports.com/blog/what-is-a-meniscus-tear-and-how-can-i-treat-it/


 CZK
CZK
 EUR
EUR
 EUR
EUR
